Birth Recovery & Postpartum Timeline
The First Weeks
We’re here to steer you through the next 12 months with a look ahead in anticipation of what’s next. This timeline identifies benchmarks in each time frame, and offers suggested reading and statistics that may help you understand exactly what is happening, both physically and emotionally. What’s most important is for you to understand what’s normal and what’s not, and when you should seek help from a professional, whether it’s a healthcare provider or lactation consultant. We’ll do that with storytelling and evidence-based support at every step of the way.
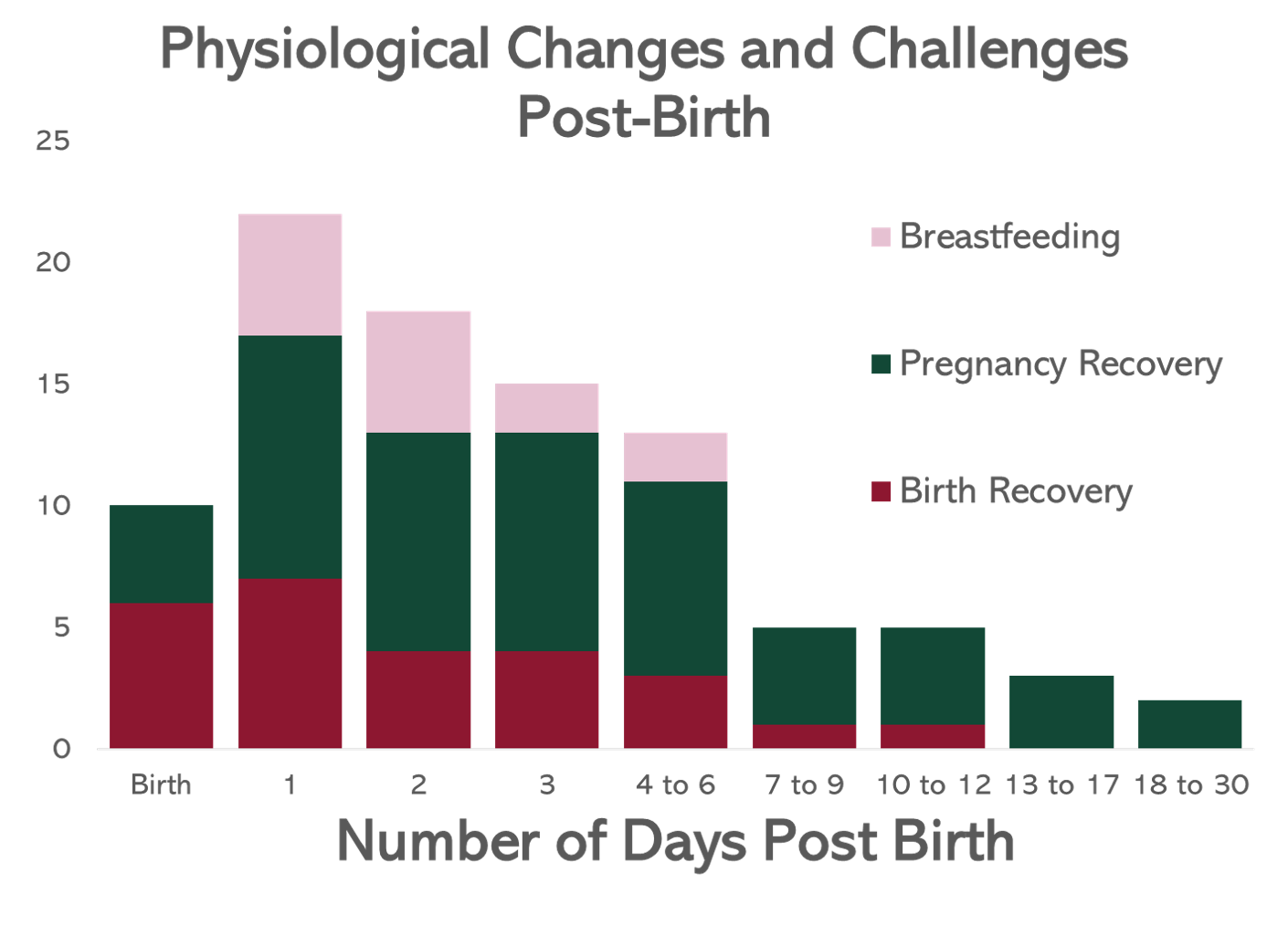
First Few Weeks After Birth: After nine-plus months of pregnancy, you are now officially on the other side, firmly planted in parenthood and the postpartum period. Each hour, each day of these early weeks is full of transitions and transformations — you are in the thick of it.
During this exceptionally fragile time you’ll recover from pregnancy and birth, initiate caring for your newborn, tackle breast or bottle feeding, and adjust to a frequent feeding schedule that is light on sleep but high on love — all while riding a hormonal roller coaster that can shock your system with its severity. If you’ve had a vaginal delivery, you might be recovering from stitches; if you delivered via cesarean birth, which involves an incision through the abdomen — severing layers of tissue and muscle — that needs proper care and internal healing that can take up to a year.
Postpartum bleeding, called lochia, starts right after birth (no matter what type of delivery you had) and can continue for up to six weeks. It might come as a surprise how intense the bleeding can be — you may find that you need to change a maxi pad specifically designed for this especially heavy flow every few hours. Rest assured the heavy volume of blood is normal and will wane in the weeks to come; to identify signs of abnormal bleeding, read “What Postpartum Bleeding Is Really Like.” Also keep in mind that you can’t use tampons during the immediate postpartum period.
If you are choosing to breastfeed, that process starts at birth and evolves over the first few weeks. (Our Breastfeeding Timeline is a must-read if you’re choosing to nurse or pump.) Colostrum is the first phase of breast milk that the body produces, followed by transitional milk that offers a newborn complete nutrition. It can take some time to feel confident breastfeeding, but patience and some troubleshooting are often all that’s needed to feel comfortable.
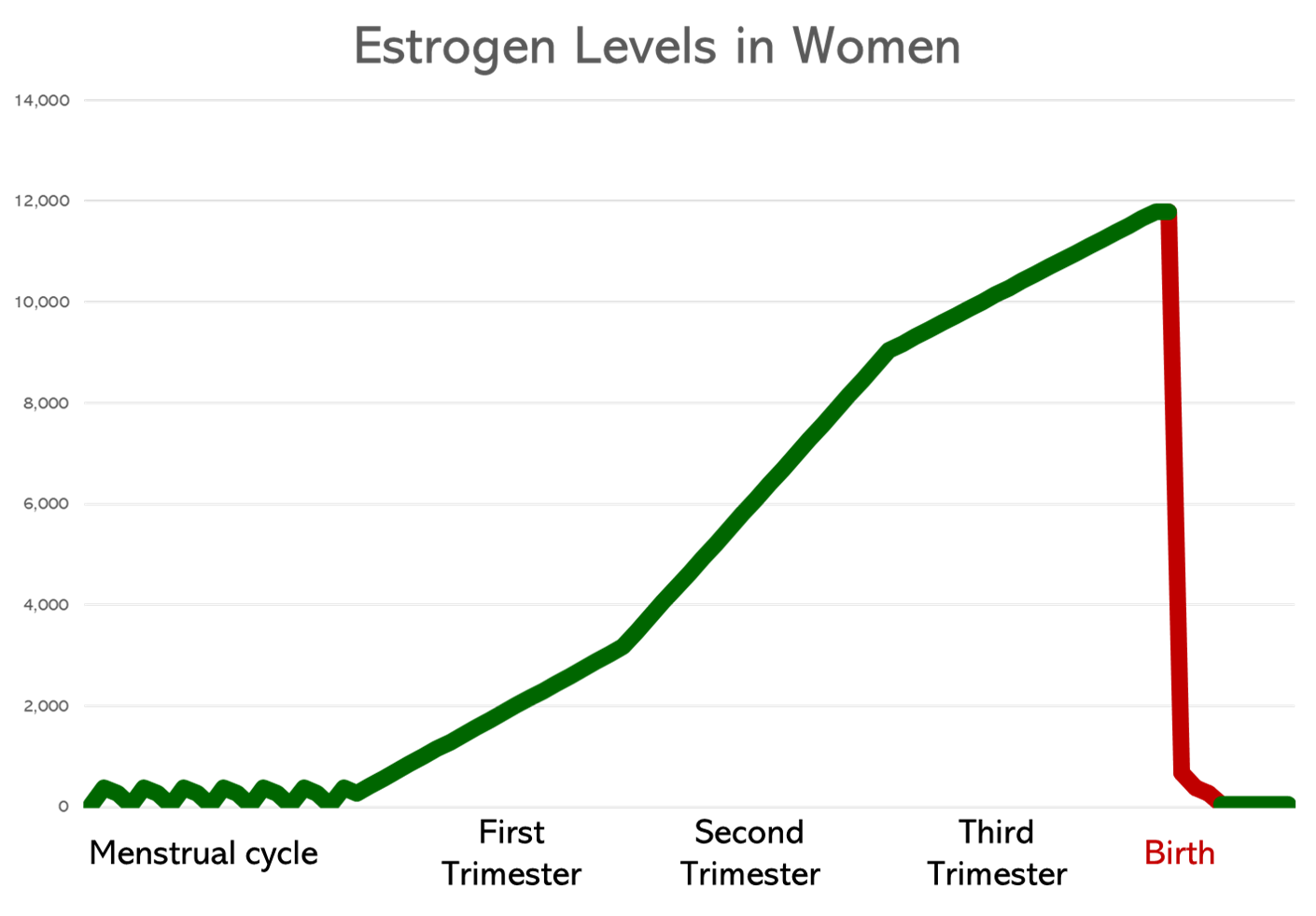
Progesterone and estrogen, hormones that were extremely elevated in pregnancy, fall dramatically upon the removal of the placenta (the source of said elevated hormone levels), enabling the body to produce breast milk. That dramatic fall — a 1,000% change in just a matter of days — can also trigger the onset of extreme postpartum emotions. For some new parents (up to 20%), this period of rollercoaster-like ups and downs can trigger postpartum depression.
This is a time to take it slow, get as much rest as you can, and ask for help whenever and wherever it’s needed.

Postpartum Bleeding
Common experiences during this period include:
+ Postpartum Emotions + Vaginal Tearing + Cesarean Birth Recovery + Postpartum Contractions See AllStage 1: 1-3 Months
This time period will bring many transitions and adjustments — your body will slowly start to heal from birth. A cesarean incision will begin to feel less tender and any vaginal stitches will have dissolved, though the perineal area may still feel painful or sore. Your body is starting to move through the recovery process from pregnancy toward its pre-pregnant state, hormones included. That includes a series of unexpected, sometimes alienating, experiences. For example, about 50% of people discover their feet have grown — permanently! — around half a size after giving birth.
Hormonally, you might still be feeling wildly-shifting mood swings — your body is still adjusting to its postpartum levels, especially if you are in the early stages of nursing, which can cause estrogen levels to be low. On the positive side, oxytocin, the “happy” hormone, is released during breastfeeding, which can relax the parent and promote bonding. Being aware of what is normal and expected, and what could be a sign of postpartum depression is critical at this stage. If you have concerns about your mental and emotional state, don’t wait for your six-week checkup to call your doctor or midwife. Our article on overwhelming postpartum emotions can help you to learn more; take the accompanying questionnaire if you have concerns.
If you are breastfeeding, the body is working to identify how much milk to produce based on specific signals, including the duration and frequency of nursing or pumping sessions. Common challenges include adjusting to the near-constant feeding schedule and milk production: Sometimes supply can seem low, and at times it can be overly abundant and cause problems with latching, engorgement and pain. Optimizing nursing positions and latching techniques to prevent sore nipples (which affects roughly 50% of people who breastfeed) can make a world of difference.
While your period still may not have returned, you can get pregnant if you’re sexually active — even if you’re breastfeeding. On average, the first postpartum ovulation occurs 45 days after birth, so it’s important to have a plan for contraception.
The six-week mark is typically when you’ll have your postpartum checkup with your care provider. Any questions about your body, how it’s healing or how you are feeling should be addressed. While it is generally thought to be the point in time when sexual activity is cleared, that is simply because any vaginal stitches will have healed. It’s important to note that just because you can have sex doesn't mean you have to — and let us mention that it can take months (and even a year) post-birth for your sex drive and emotional state to be truly ready for it. Why? Hormonally, your body’s libido is all tied up in breastfeeding and pregnancy recovery, with low estrogen levels causing vaginal dryness, and prolactin, a nursing hormone, counteracting arousal. The postpartum checkup is also critical for identifying any post-birth conditions like diastasis recti (abdominal muscle separation, a condition that affects 60% of people six weeks after birth and 30% at one year after birth) or incontinence (which can affect one-third of first-time parents and be an indicator of pelvic prolapse), both of which can be treated with physical therapy if identified early.
You might be getting ready to return to work (25% of the U.S. population returns to work within 14 days, and only 16% has 12 weeks paid leave), which means you’ll have to sort out how to handle feeding. If you’re nursing, that means familiarizing yourself with your breast pump if you haven’t already, and connecting with your point person — whether an HR manager or supervisor — to see how you’ll be accommodated at your workplace.
Postpartum Headaches & Preeclampsia
Common experiences during Stage 1 include:
+ Post-Pregnancy Body Changes + Postpartum Emotional Deluge + Sleep Deprivation + Increasing Milk Production See AllStage 2: 3-6 Months
By the three-month mark, most vaginal delivery wounds will be healed, though it’s common to still have sensitivity or discomfort, or feel tender at the site of stitches — especially if you had an episiotomy or third- or fourth-degree tearing. If you’re breastfeeding, you might feel like you’ve hit your stride and identified techniques that work best for you and your baby.
Around four months, you will notice that your hair is falling out. A lot. That’s because during pregnancy you didn’t shed any — all those strands are now falling out, often in large clumps around the hairline, leaving telltale “baby fuzz” at the temples and above your ears. Don’t worry, you’re not going bald and this is completely normal.
Remember your period? It can return any time now, though everyone’s cycle is different and the amount of time you breastfeed can prolong the time till it returns. It’s worth noting that the first few periods post-birth can be heavier and particularly crampy, especially if you are breastfeeding.
Mentally and emotionally, hopefully you are feeling more even-keeled due to hormones that have readjusted back to pre-pregnancy levels. If you aren’t, don’t hesitate to reach out to a healthcare professional for support and guidance.

Postpartum Urinary Incontinence
Common experiences during Stage 2 include:
+ Post-Pregnancy Body Changes + Sleep Deprivation + Increasing Milk Production + Breast Size & Breastfeeding See AllStage 3: 6-12 Months
Your body has come full circle, with your uterus back to pre-pregnancy size at around the nine-month mark and ovulation nearing regularity again. If your period hasn’t returned yet, it will likely arrive before your baby’s first birthday. If you find your sex drive isn't quite at full steam, rest assured that you’re not alone: Breastfeeding, if you’ve continued this long, can cause your hormone levels to rest decidedly in the not-in-the-mood-for-sex zone, and can also restrict natural lubrication. Also, if you had a vaginal birth that required stitches, it still might not feel comfortable to have sex, and that’s totally normal (and will get better!). Take the time you need and seek the kinds of connections with your partner that feel meaningful so you can slowly tilt your intimacy levels back to what feels right for you.
Pelvic floor strength can take some time to come back, but by this point you shouldn’t be struggling with incontinence. If you are, seek pelvic floor therapy to help strengthen the core muscles which support your bladder control.
If you had a cesarean birth, you might find that your abdominal strength is still not quite back to your “normal.” Seeking the right kind of postpartum exercises to help strengthen your core can help you regain strength and alleviate any secondary issues, like back pain. Sensation around your incision may slowly start to come back, but it’s not uncommon for it to take longer than a year (or not return at all, due to the severing of nerve tissue).
If you’re still breastfeeding around the one-year mark (which roughly 36% of women are), you might be thinking about weaning. Take a look at our Breastfeeding Timeline for more information on decreasing production and the emotional effects associated with weaning.
You might be back to your pre-pregnancy weight, and you might not be. On average, women who gained the recommended amount of weight during pregnancy will find they are still 2-5 pounds over their pre-pregnancy weight; if you gained more than that, it can be closer to 10-20 pounds. Health is the most important thing to remember here — you spent nearly a year growing a baby, and it might take a year or more to find balance in your body.

Diastasis Recti (Abdominal Separation)
Common experiences during Stage 3 include:
+ Sleep Deprivation + Breastfeeding & Food + Increasing Milk Production- Choosing a selection results in a full page refresh.
- Opens in a new window.



-v1695651502205.png?1000x1229)
